Yes. The US Centers for Disease Control and Prevention (CDC) recommended that dentists provide prediabetes and diabetes prevention care. This should include at least awareness, education, and screening.
To summarize the role of dentistry in this area, take this quote from an article titled “Prediabetes and Diabetes Screening in Dental Care Settings: NHANES 2013 to 2016” (Estrich, 2016).
Screening for prediabetes at dental visits has the potential to alert an estimated 22.36 million adults of their risk for prediabetes or diabetes… Screening for prediabetes and diabetes during dental visits has the potential to raise patients’ awareness of diabetes risk and prevent prediabetes from progressing to diabetes. For some patients, the dental visit may be the only point of contact with the health care system, which heightens the importance of including diabetes risk assessment for patient well-being.
But wait…
Doesn’t the US have the best primary care support for prediabetes and diabetes?
The short answer is no. There is plenty of research showing just the opposite.
One of these studies is a recent survey of US primary care physicians (PCPs) done by researchers from Hopkins (Tseng, 2019).
Here are a few problems that they listed:
- “Despite strong evidence and national policy supporting type 2 diabetes prevention, little is known about type 2 diabetes prevention in the primary care setting.”
- “PCPs had limited knowledge of risk factors for prediabetes screening, laboratory diagnostic criteria for prediabetes, and management recommendations for patients with prediabetes.”
- “Only 36% of PCPs refer patients to a diabetes prevention lifestyle change program as their initial management approach…”
- “… while 43% discuss starting metformin for prediabetes.” (PCPs immediately resort to metformin or other prescription medications, not lifestyle.)
- “PCPs believed that barriers to type 2 diabetes prevention are both at the individual level (e.g., patients’ lack of motivation) and at the system level (e.g., lack of weight loss resources).” (PCPs blame the problems on patients and insurance companies.)
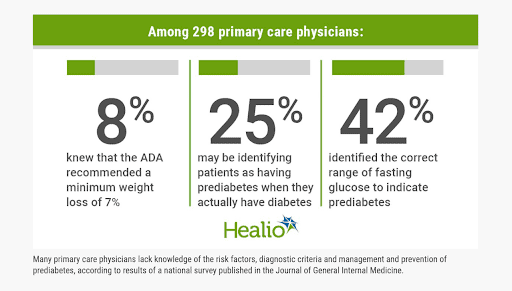
Source: Michael E. Many PCPs lack knowledge about prediabetes, survey finds. Healio website.
This is where dentists come in, in terms of the fight against the prediabetes and diabetes epidemic
Dentists are in a unique position in terms of public health.
Why?
Because dentists see peoples’ gums all day.
What do gums have to do with it?
It may not be a widely known fact, but inflamed, reddish, and bleeding gums are early warning signs of prediabetes.
But you may think, “it’s ‘only’ prediabetes.”
Is prediabetes the same as diabetes?
Don’t let the “pre” in prediabetes fool you. Prediabetes, metabolic syndrome, or insulin resistance are all parts of the same disease process as type 2 diabetes.
This disease process leads to over 75% of cardiovascular (CV) inflammation and arterial plaque. By far, this is the leading cause of heart attacks (the #1 cause of death), strokes (the #1 cause of permanent disability), blindness, kidney damage, among other things.
Is it ok for a dentist to order lab tests for prediabetes or inflammation? Are they the doctors now?
Unfortunately, similar quotes from medical doctors are common. They blatantly imply that dentists are going outside their professional practice roles if they provide prediabetes prevention services. I’ve even witnessed renowned leaders in preventive medicine making similar comments.
Sometimes, the medical community focuses too much on top-down approaches to care. This physician elitist approach results in the loss of prediabetes preventive services.
Here is a great article, written by a dentist who described how his help was dismissed in a CV emergency on a plane (Pynn, 2010). His situation evoked famous quotes from the movie “The Hangover,” like, “Do you mind if I take a look. I’m actually a doctor.” “Yeah?… you’re just a dentist.” “You’re a dentist. Don’t try and get fancy.”
This negative impression on dentists and their profession is only the tip of the iceberg. The bigger impact is the damage being done to our patients’ and the public’s health.
Dentists are not PCPs. Should dentists attempt to help fill the void of informed PCPs?
In the US, the CDC and NIH (National Institutes of Health) said yes. In the UK, the Royal College of Surgeons has recommended the same thing (Winning, 2015).
Other groups are also supporting the big role of dentists. For instance, the American Academy of Periodontology and the European Federation of Periodontology have these specific recommendations for oral health practitioners (Tonetti, 2013):
- Practitioners should make patients aware of the evidence that periodontitis is a risk factor for developing CV disease.
- Periodontitis patients with comorbidities (high blood pressure, increased body fat, tobacco use, etc.) should see their doctor at a minimum yearly or be referred to other doctors.
- Practitioners should address risk factors in the dental setting and context of periodontal disease (e.g. diet, exercise, smoking cessation, blood pressure, and glucose checks).
Are there any detailed resources or specific programs to help dentists in prediabetes management?
Yes, and this is where NDEP and PPOD enter the picture.
What is NDEP?
NEDP (National Diabetes Education Program) is a joint effort of 200+ federal, state, and private sector partners. It was established in 1997 by the CDC and NIH to improve prediabetes and diabetes preventive care (awareness, screening, and education) and to decrease such disease impact in the US.
Source: CDC. NDEP page. CDC website.
Some program recommendations you can find in NDEP are based on data provided by government surveys, like the National Health and Nutrition Examination Survey (NHANES), and partner organizations, like the American Diabetes Association, American Academy of Nurse Practitioners, Academy of Nutrition and Dietetics, and American Association of Diabetes Educators (Siminerio, 2018).
What is PPOD?
The PPOD program is a core component of NEDP. It’s a collaborative team approach for pharmacists, podiatrists, optometrists, and dentists; hence, the acronym PPOD (pharmacy, podiatry, optometry, and dentistry).
The program aims to:
- Engage many health care providers in a team approach to treat patients with diabetes;
- Reinforce consistent diabetes message across four disciplines—pharmacy, podiatry, optometry, and dentistry;
- Reinforce self-management, healthy habits, and periodic screening;
- Focus on PPOD providers treating patients as well as providing educational services;
- Recognize that PPOD providers are often the first (and sometimes the only) point of care for some patients.
We can access things about the PPOD program on CDC’s PPOD page. The page primarily talks about how PPOD care providers are well-positioned in diabetes prevention and management. It also provides toolkits (including this PPOD document as shown in the image below), training courses, and other resources where PPOD practitioners can learn how they can all work with each other.
Source: Rodgers P, Bennett PW, Frisch DR, et al. PPOD guideline. CDC website.
PPOD care programs include not only the usual care for the individual specialty but also other components, like the following ABCS:
- A1c for blood glucose control;
- B for blood pressure control;
- C for cholesterol control;
- S for smoking or tobacco cessation.
Will taking part in the PPOD program create an extra burden to dentists?
Prediabetes preventive care is not volunteer care. It is more valuable to dental patients—and the country—than most medical and dental care.
When dentists get over the common hesitation to “go outside their lanes” and join the prediabetes prevention team, usually, they assume incorrectly that these are not valid, value-laden services for which they should charge.
Even though preventive services require no extra office space, minimal extra time for dentists or hygienists, minimal equipment, and minimal process time, these services are billable. Failure to generate any revenue through services is a great way to assure failure in providing them. And failure to provide these services is already hurting our patients and communities.
Given the guidance and recommendation from expert groups, will there still be questions about dentists’ role in terms of prediabetes and diabetes prevention?
Let’s hope not. You can post your comment on our forum or YouTube channel, and tell us what you think.
If you found this article helpful and want to start taking steps toward reversing your chronic disease, Dr. Brewer and the PrevMed staff are ready to serve you no matter where you’re located.
To find out more, schedule a consult here: prevmedhealth.com
References
Centers for Disease Control and Prevention (CDC). National Diabetes Education Program. CDC website. https://www.cdc.gov/diabetes/ndep. Page last reviewed June 7, 2018. Accessed September 23, 2020.
Centers for Disease Control and Prevention (CDC). Working Together to Manage Diabetes: A Toolkit for Pharmacy, Podiatry, Optometry, and Dentistry (PPOD). CDC website. https://www.cdc.gov/diabetes/ndep/toolkits/ppod.html. Page last reviewed February 19, 2016. Accessed September 23, 2020.
Estrich CG, Araujo MWB, Lipman RD. Prediabetes and Diabetes Screening in Dental Care Settings: NHANES 2013 to 2016. JDR Clin Trans Res. 2019;4(1):76-85. doi:10.1177/2380084418798818
Michael E. Many PCPs lack knowledge about prediabetes, survey finds. Healio website. https://www.healio.com/news/primary-care/20190913/many-pcps-lack-knowledge-about-prediabetes-survey-finds. Published September 13, 2019. Accessed September 23, 2020.
Pynn BR. You’re Only a Dentist… Oral Health website. https://www.oralhealthgroup.com/features/you-re-only-a-dentist. Published June 1, 2010. Accessed September 23, 2020.
Rodgers P, Bennett PW, Frisch DR, et al. Working Together to Manage Diabetes: A Guide for Pharmacy, Podiatry, Optometry and Dentistry. https://www.cdc.gov/diabetes/ndep/pdfs/ppod-guide.pdf. Published January 2014. Accessed September 23, 2020.
Siminerio LM, Albright A, Fradkin J, et al. The National Diabetes Education Program at 20 Years: Lessons Learned and Plans for the Future [published correction appears in Diabetes Care. 2018 Mar 16;:]. Diabetes Care. 2018;41(2):209-218. doi:10.2337/dc17-0976.
Tonetti MS, Van Dyke TE, working group 1 of the joint EFP/AAP workshop. Periodontitis and atherosclerotic cardiovascular disease: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Clin Periodontol. 2013 Apr;84(4 Suppl):S24-9. doi: 10.1902/jop.2013.1340019.
Tseng E, Greer RC, O’Rourke P, et al. National Survey of Primary Care Physicians’ Knowledge, Practices, and Perceptions of Prediabetes. J Gen Intern Med. 2019 Nov;34(11):2475-2481. doi: 10.1007/s11606-019-05245-7.
Winning L, Linden G. Periodontitis and systemic disease. BDJ Team. 2015;2:15163. https://doi.org/10.1038/bdjteam.2015.163.