Today we’re going to talk about stopping statins. It is an interesting topic since some folks think it is safe to stop statins regardless of how long they were used. However, there are some things to consider before making that decision.
An Introduction Story
I have a friend, he’s about 60 years old. His father died of a heart attack when he was 51. My friend had a plaque, but he slowed it down, then reversed it. He decreased the size of the plaque, then hardened it.
He felt like he was in good shape. So, he decided it was time to stop taking his statin. He did, and in less than a year off the statin, his plaque both softened and started growing.
As a side note, a study in the Journal of the American Heart Association about people who have stopped statins post-plaque comes to mind. That is because, there’s a lot of conflicting information in the literature. Or maybe not, if you understand the mechanisms behind statins.
Why Do People Stop Taking Statins?
So, what are the reasons for stopping statins? Some are:
• Side effects: fatigue, muscle soreness, malaise (a medical term for feeling bad), and increased blood glucose.
• Statins can move you down the diabetic highway if you’re insulin resistant.
• You are switching to another statin. You may realize that you’re on the wrong statin. You may be on something like Lipitor, and you’re insulin resistant. It’s not having a meaningful anti-inflammatory impact.
• Cost
• Fear: most of my patients are baby boomers, and the baby boomer generation does not like to take medication. It’s not so much a fear; it’s just an emotional thing about wanting to be whole, healthy, and natural. In their eyes, anything like medication is a bad thing.
• You don’t believe Rory Collins and the cholesterol treatment trial lists.
• You’ve seen too many YouTube videos on the dangers of statins.
Within the Cholesterol Treatment Trialists Collaboration, there’s been debate about statin treatment between the British Medical Journal and Lancet for at least six years. Those are the two major medical science journals in England.
Rory Collins is from The Lancet Group. He’s been involved in debate about the British Medical Journal publishing things that say statins are dangerous for you. However, Rory Collins and his group are saying they’re dangerous, but they’re not as bad as going statin-free.
They did a meta-analysis, and yes, myopathy can happen in a relatively good number of people. Just so you understand, myopathy, or cardiomyopathy, is a disease that makes it hard for the heart to pump blood to the rest of the body. It can result in heart failure.
Now back to the data. 10,000 people, either low-risk or high-risk were followed around for 5 years. Turns out, myopathy was associated with statin treatment. Even more, this was severe myopathy, which can kill you.
Also, increasing insulin resistance was seen. Researchers listed the findings as new-onset diabetes. Most researchers would say it doesn’t start diabetes if you don’t have it. However, it may move you down the diabetic highway.
Another important finding, you can also get hemorrhagic stroke- what was thought several years ago.
Worst-case scenario there were 115 bad outcomes from statins in 10,000 people. Another way to look at, 10,000 low-risk people would suffer 500 heart attacks or strokes which may be fatal.
Conversely, if this were a high-risk group, there would be 1,000 heart attack or strokes. That’s what Rory Collins and his group were saying.
More Evidence
Let’s discuss the study I mentioned in the American Journal of the American Heart Association in August 2017. They said it’s dangerous to stop your statins after a stroke.
For the record, I want to mention another study to show that this is more complex than it seems. This was a study done in 2004. The headline says, “Stopping Statins in the Short Term is Okay for Stable Patients.” We’ll come back to this study later.
Let’s go through the study published in the Journal of the American Heart Association on August 2, 2017, “Utilization of Statins Beyond the Initial Period after Stroke and One Year Risk of Recurrent Stroke.”
The results showed a significant increase in recurrent stroke in patients who stopped their statins. Among the 45,151 ischemic stroke patients meeting the criteria during the 90 – 180 day period, 7% were on reduced therapy, and 18.5% were not on any treatment compared to statin-intense therapy.
It’s less than a 5% probability this would happen out of random chance. When we review the actual numbers, you’ll see that the possibility was less than one-hundredth of one percent.
Their conclusion was, “discontinuation of statin therapy between 3-6 months after an ischemic stroke is going to increase your probability of having another stroke”.
Here is one of the tables from this study. It shows a dip in recurrent stroke and ischemic stroke. One of the problems with this study is they didn’t clearly define the difference between a recurrent stroke and a secondary ischemic stroke. They only showed that you’re more likely to have a “stroke”.
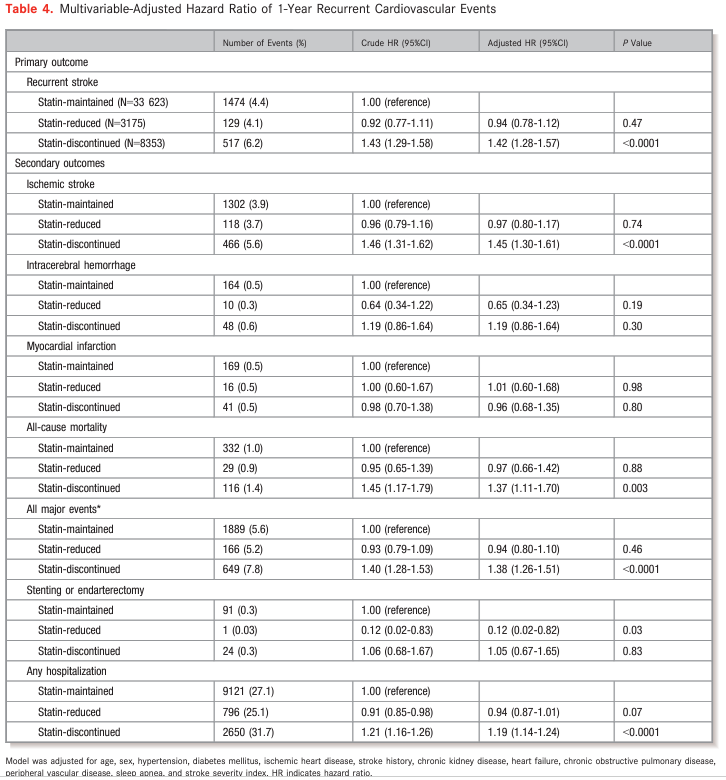
Of 1,474 strokes from 33,623 people who maintained statin therapy, those that discontinued the statins totaled 8,353. That said, of those who discontinued, 1500 (4.4%) had strokes. Among the 8,000 that stopped the statin, there were 517 strokes or 6.2%. The probability of that difference is less than one-hundredth of one percent.
I don’t recommend that post-stroke patients stop their statins because there are still problems with this study. Sadly, this study has the same problem that many other scientific studies have: the exclusion criteria issue. This was in a Taiwanese registry for strokes. It was a retrospective study- meaning they took information from strokes that had already occurred and tabulated it.
Let’s look at the exclusion criteria. First, 32,000 were excluded due to having a recurrent stroke within 180 days after discharge.
They’re saying you often get one stroke after another in rapid succession.
It’s true. A quarter of strokes happen in people that have already had one. The authors said, “let’s be conservative and rule that group out “. They may have good reasons for exclusion criteria, but it’s only possible to tell if they describe them-which they didn’t.
Here’s where it becomes apparent: when the rest of the scientific medical community starts debating the quality of that study and the quality of the logic that’s revealed in the paper.
What were the exclusion criteria?
• First, follow up less than 180 days. That makes sense if they are excluded because they are receiving hemodialysis. Hemodialysis is a major destabilizer.
• 66,000 participants were excluded due to not having antiplatelet or anticoagulant within 180 days. Again, it’s reasonable because if you didn’t have antiplatelet treatment, it’s more likely to be the reason for a recurrent stroke than statins.
• 120,000 were excluded because they didn’t have a statin, or a low-dose statin, within 90 days after the hospital discharge.
We have to give the authors credit that they knew what they were doing and had sound logic behind it, but I’m not fully hearing it.
Every study has its problems. But based on this, I’m not going to recommend my post-stroke patients stop their statin.
Why did this happen? Why do we see two studies – one that says it’s okay to stop your statin and another that says it’s not?
Because the two studies, and their results, are totally reasonable, compatible, and expected.
The Safety of Statins
The study showed safety was with stable patients. The study showing hazard was with patients that had had a recent stroke. Plaque instability is systemic. Remember, I did a video recently about the theory of vulnerable plaque.
There have been companies and startups all based on the assumption that you could and that one plaque is creating danger for the patient. Those companies didn’t make it, or they morphed into something else.
That theory is rapidly dying. Here’s why: plaque instability is systemic. Therefore, if there’s no such thing as a single vulnerable plaque, then where there’s one unstable plaque, there’s a whole arterial tree full of unstable plaques.
Likewise, if your plaques are stable and healthy (relatively speaking), they will remain that way. That said, going by a study of people who are strict and healthy, it’s okay to stop statins for a short period. It certainly appears that way.
But if you’re unstable and have evidence of a hot plaque, more hot plaques are waiting to cause damage.
If you found this article helpful and want to start taking steps toward reversing your chronic disease, Dr. Brewer and the PrevMed staff are ready to serve you no matter where you’re located.
To find out more, schedule a consult here: prevmedhealth.com
REFERENCES:
1. https://prevmedhealth.com/do-statins-prevent-heart-attacks/https://prevmedhealth.com/the-demonization-of-statins/
2. https://prevmedhealth.com/stopping-statins-is-it-safe/
3. https://prevmedhealth.com/how-to-test-for-cardiovascular-inflammation/
4. https://prevmedhealth.com/olive-oil-and-cv-inflammation/
5. https://www.ahajournals.org/doi/10.1161/01.CIR.0000145140.06171.3D
6. https://pubmed.ncbi.nlm.nih.gov/27616593/
7. https://pubmed.ncbi.nlm.nih.gov/28768645/