The immune system is involved with the body’s process of injury repair. It kills, digests, and removes pathogens.
Ironically, the immune system also creates inflammation while protecting and healing the body. It can attack body tissues if it doesn’t recognize them or if body tissues are in the wrong locations.
For instance, with rheumatoid arthritis, the immune system attacks joint tissue. In lupus patients, antibodies to the cell’s nucleus indicate another internal target of the immune system’s attack. In Hashimoto’s thyroiditis and inflammatory bowel disease, the immune system targets the thyroid gland and intestines, respectively.
The artery walls are taking “friendly fire” from the body’s immune system, and we call such events as cardiovascular (CV) inflammation. This, along with other inflammatory diseases (like rheumatoid arthritis) increases the risk of heart attack and stroke.
The Layers of the Artery
Before we connect CV inflammation with heart attacks and strokes, let’s define first the 3 layers of the artery.
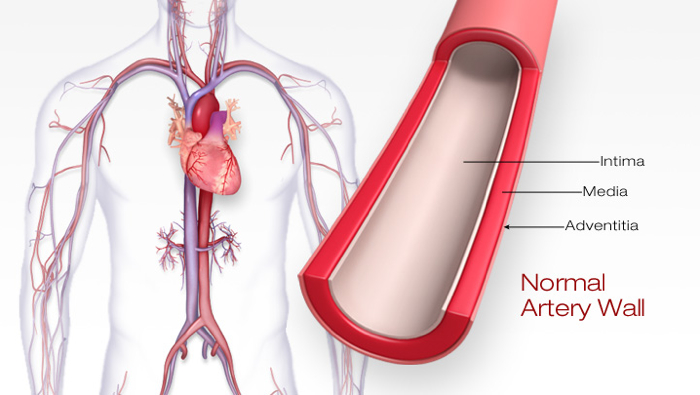
Layers of the Artery. Source: American Stroke Association. Atherosclerosis and Stroke. American Stroke Association website.
Intima
The intima is a thin layer lining the artery wall. It includes a single-cell layer called the endothelium. (The endothelium is the largest organ in the body, lining all 100,000 miles of vasculature in adults and every other organ in the body.)
Upon closer look, you’ll see the intima being lined with hair-like structures called the glycocalyx. The glycocalyx provides an increased surface area for the exchange of carbon dioxide, nutrients, and waste products. Thus, it appears to be the major area of metabolic activity in the arteries.
Why are we mentioning glycocalyx? That’s because it’s a weak spot in the intima. Damaged glycocalyx (which means damaged intima too) plays a central role in plaque formation and CV inflammation.
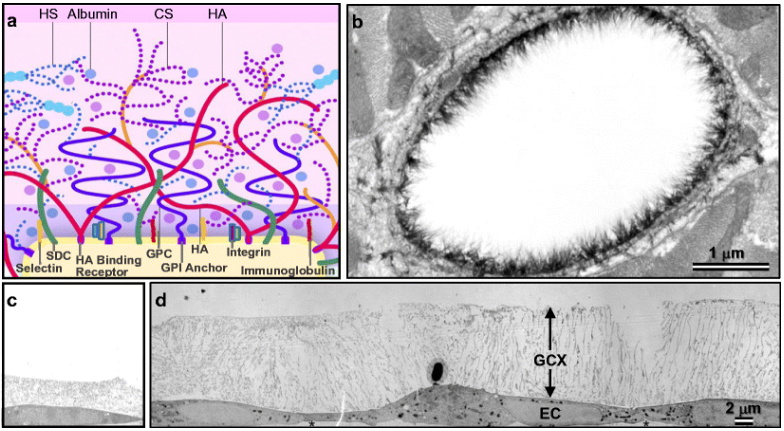
Figure A above is a representation of the glycocalyx (the hairy structures lining the intima), showing some of its biological components. Figure B shows a larger picture of the artery wall, using a STORM method microscopy. An injured, thin glycocalyx is shown in Figure C, while a healthy, thicker glycocalyx is shown in figure D. Source: Oshima K, Haeger SM, Hippensteel JA, Herson PS, Schmidt EP. More than a biomarker: the systemic consequences of heparan sulfate fragments released during endothelial surface layer degradation (2017 Grover Conference Series).
Media
The media is the smooth muscular layer of the artery walls. This layer provides strength, structural integrity, and the gentle elastic motion of contraction and relaxation required to pump blood through the body.
The media’s principal function is to regulate the caliber of the blood vessels. Excessive vasoconstriction leads to high blood pressure. On the other hand, excessive vasodilation leads to low blood pressure.
Tunica Adventitia
The last layer of the artery is the tunica adventitia. This is the hard, white, sinewy layer composed mostly of collagenous and elastic fibers.
The adventitia provides a limiting barrier and holds the rest of the arterial wall together. Without the adventitia layer, arteries would disintegrate under pressure.
Atherosclerosis, Inflammation, and Heart Disease
You may already have heard the term “atherosclerosis.” It means a build-up of plaque in the artery wall that could restrict blood flow. It comes from the Greek roots “athero” (meaning “artery”) and “skleros” (meaning “hardening” or “scarring”).
Arterial plaque is made up of fats, cholesterol, and other substances that get stuck within the artery walls. Many assume plaques line the lumen (the hollow space of the artery) like hairs lining the inside of a shower drain where water flows. This assumption is wrong, though, as plaques are like the acne bumps lining the walls.
Plaque can be a problem as it plays a big role in most heart attacks, strokes, blindness, and dementia. That’s why there’s so much emphasis on curbing fats and cholesterol to reduce heart diseases.
However, the problem goes beyond plaque. A bigger culprit looms with inflammation, the immune system’s response to any damage in the body.
Inflammation Starts with Injured Intima
Endothelial cells (like those found in the intima’s glycocalyx) are permeable. This is important because the artery is a live vessel. And like other live tissues in the body, the artery needs nourishment.
Because the endothelial cells are permeable, they also provide ample space for other components—like pathogens, immune cells, and oxidized LDL cholesterol—to pass through.
Here’s the problem. Once oxidized LDL particles penetrate an injured glycocalyx or intima, they could get trapped in the space between the intima and media layer, leading to plaque build-up and eventually inflammation.
Plaque attracts the attention of immune cells called monocytes to the wall’s surface, which kicks off a series of inflammatory events. Once immune cells find their way to the location of plaque, they will release several enzymes (like Lp-PLA2 and myeloperoxidase) to destroy that plaque.
Monocytes are then converted to pathogen-destroying cells called macrophages. The byproducts of macrophages’ actions are foam cells and fatty streaks, which are inflammatory (further adding fuel to the fire).
Simultaneous to the above processes, other chemicals are released as well. Those that attract more immune cells to the area of inflammation are called cytokines (“cyto” means “cell,” and “kines” means “attractants”). Cytokines will drive inflammation further within the area.
As the inflammatory process ensues, a pool of liquid material forms. This pool will consist of immune cells, cytokines, debris, and necrotic material formed by the immune processes. This pool eventually grows to become soft plaque.
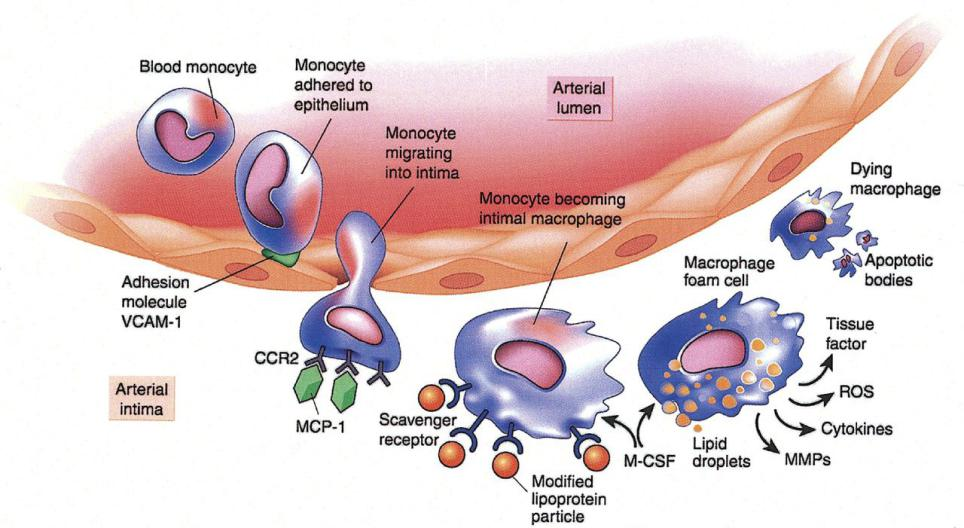
The biology of atherosclerosis initiation, progression, and complications. Source: Jaffer FA, Libby P, Weissleder R. Molecular and cellular imaging of atherosclerosis: emerging applications.
Soft Plaque Rupture
Soft plaque includes proteins, oxidized LDL, glycoproteins (proteins with carbohydrate chains), and the necrotic byproduct of cell destruction. It is like the sticky white substance you would find inside a large acne lesion.
A calcific cap forms over soft plaque. The necrotic material also attracts enzymes that can weaken both the arterial wall and that thin, fibrous cap that prevents necrotic material from seeping into the bloodstream.
Over time, soft plaques could then rupture like a pimple. This happens because of the shear stress of the blood hitting the lesion 24 hours a day and the continued weakening of the arterial wall from the newly attracted enzymes.
Clot Formation
If the cap breaks, and soft plaque ruptures, enzymes are released into the bloodstream. Some enzymes can activate blood platelets to form a thrombus or blood clot. (This process is the same with platelets forming a protective scab over a wound.)
Unfortunately, clots are dangerous. If clots are not dissolved, they can break off the original site and get pushed into the smaller vessels. The clots can also grow so large at the site of origin that blood flow can be stopped completely (Meng, 2015).
Worse, large clots can block blood flow to the tissue, starving it of oxygen and killing it. If the oxygen-starved tissue is in the heart, the result is a heart attack. If the oxygen-starved tissue in the brain, the result is a stroke.
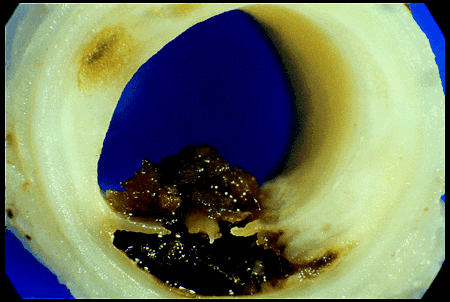
Clot formed from hot plaque.
Moreover, dying heart tissues create chaotic heartbeats or fibrillation. Without coordinated beats, the pump function of the heart disappears.
This happened to renowned broadcast journalist Tim Russert. His body stopped. When blood flow to his brain ceased, Russert lost consciousness. He never woke up.
The bad news is that this tragedy is still happening frequently in the US. Heart attacks occur every 38 seconds—half result in sudden death.
If you’d like to learn whether it’s possible to reverse arterial plaque, do check our other article titled “Reducing Arterial Plaque – Is It Possible?”
What Drives CV Inflammation?
Prediabetes
The most common driver of CV inflammation (as well as heart attack and stroke) is prediabetes (also called insulin resistance or metabolic syndrome).
It’s associated with aging or unhealthy fat stores. It dramatically increases the growth rate of plaque within the artery walls.
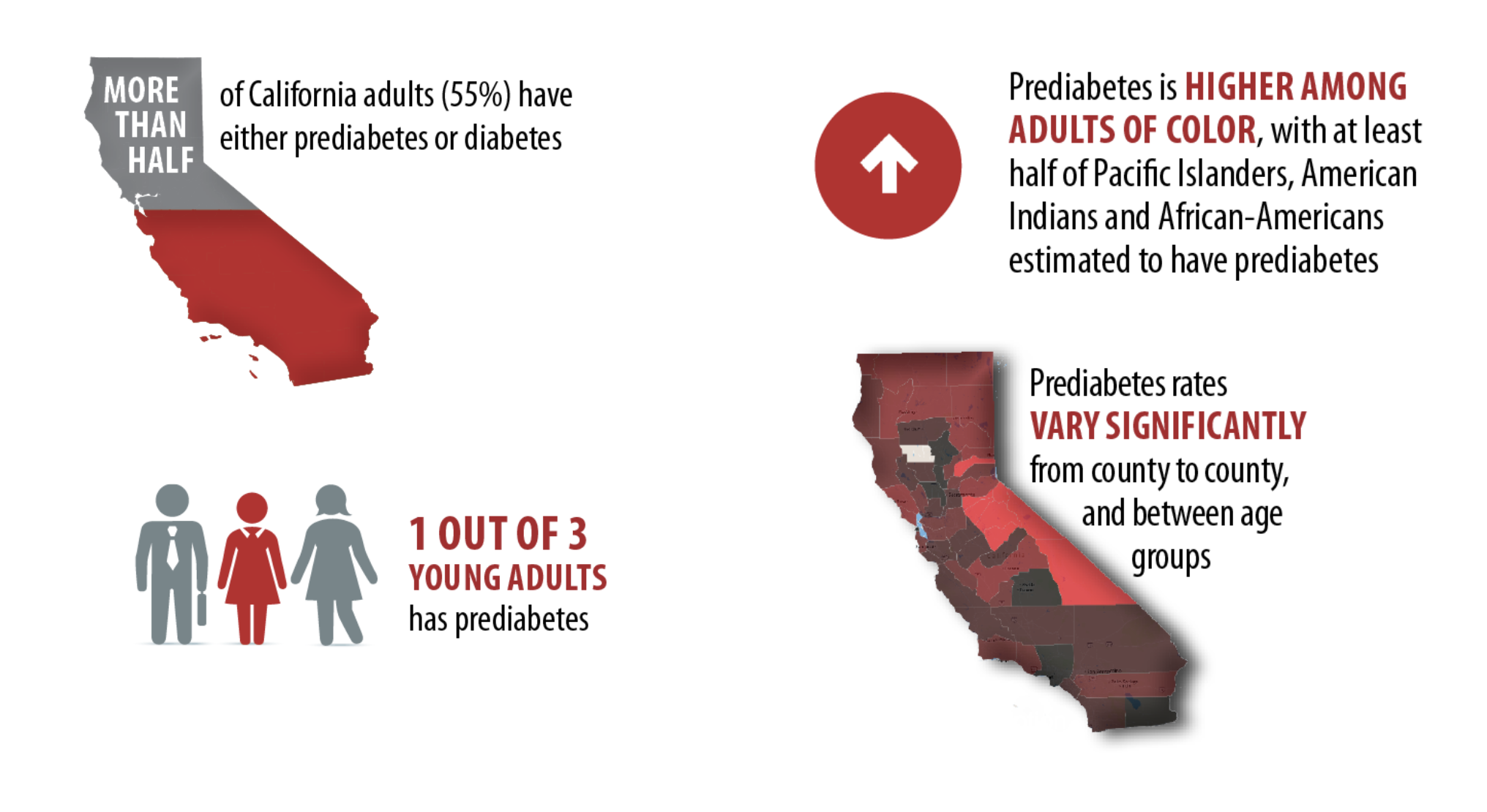
In 2017, the CDC said there were over 84 million adults in the US with prediabetes. However, 90% of these people don’t know they are prediabetic (CDC, 2017).
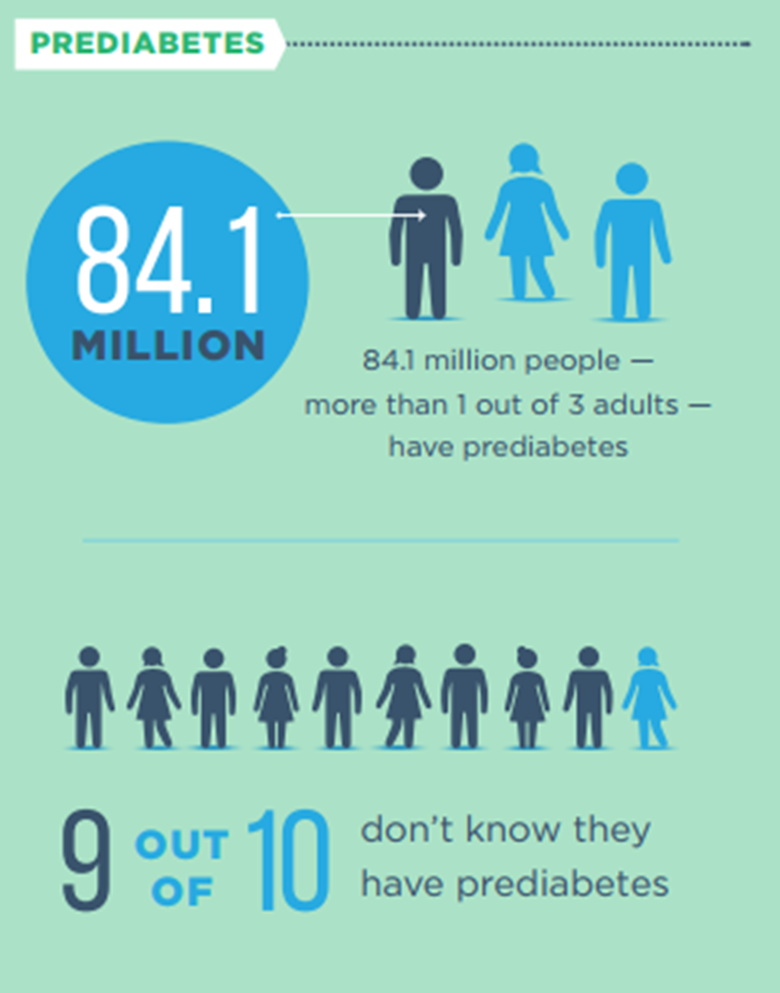
The year before, UCLA reported that over half of all adult Californians have prediabetes (Babey, 2016). This makes the above CDC’s estimates conservative. That could be largely because CDC based its findings only on fasting glucose and hemoglobin A1c. Both tests have high false-negative rates, even when used together (Kraft, 2008).
Oxidation
Oxidation is another significant driver of the inflammatory process.
The oxidation process gives humans significant advantages in terms of energy. We can extract 36 units of energy from a glucose molecule. That compares to only 6 energy units derived by more primitive species such as yeast.
This human ability to transport and use oxygen does give us extra power. However, in return, this oxygen metabolism exacts a toll of increased oxidation as we age. As a matter of fact, oxidation is the essential force described in one of the most popular theories of aging—the mitochondrial theory.
In the mitochondrial theory of aging, the furnaces of the cell (the mitochondria) slowly decline because of chronic oxidation damage. This oxidation’s role in aging is what drove the decades-long focus on supplements and antioxidants.
The Inflammation Lab Tests
There is no single definitive test for CV inflammation. But there are combinations of tests (panels) that can help measure the inflammatory processes I described above.
One example is the CV inflammation panel from Cleveland Heart Lab, now owned by Quest Labs. They include CRP, MACR, Lp- PLA2, and MPO (Brewer, 2020). If we are to use these tests effectively, it is important to understand the analyte in these panels and their relationship to the inflammatory process.
CRP (C-Reactive Protein)
CRP is a protein made by the liver in response to multiple inflammatory challenges. When the body fights inflammation, the liver makes CRP. That includes inflammation within the walls of the arteries.
Although some researchers get a CRP analysis done alone in studies, we do not recommend using it alone for an individual patient assessment.
Why?
Because there are too many false positives and negatives to relying on CRP alone for personalized CV care. For example, some studies have shown that 2 days after a flu shot, two-thirds of us will have an elevated CRP.
Because of the common false positive results one can get from a CRP test, you should include the other inflammatory tests I listed below.
MACR (Microalbumin Creatinine Ratio)
Another test, MACR measures the amount of a protein called albumin in the urine.
There are about 1 million microscopic filters in each kidney. They filter waste materials from the blood into the urine. The membranes in those filters consist of the intima or lining of the arteries. Usually, the intima membrane keeps proteins such as albumin. If the intima is damaged, albumin leaks into the urine.
Furthermore, damaged intima also leaks LDL. So, if albumin is leaking into the urine, LDL is likely leaking into the artery wall.
Lp-PLA2 (Lipoprotein-associated Phospholipase A2)
Monocytes slip through the endothelium and into the intima-media space. When these monocytes become activated, they transition into slightly different cell types called macrophages.
Macrophages continue to grow. They become scavengers, looking for pathogenic material to destroy and consume. These cells then join other activated macrophages, forming foam cells and fatty streaks. As this process continues, the cells release enzymes, including the Lp-PLA2 enzyme, which is used to destroy and digest cellular trash.
Since these enzymes only appear when the cell-destruction process is active, the higher the concentration of Lp-PLA2, the higher the likelihood a patient is fighting active atherosclerotic disease.
MPO (Myeloperoxidase)
Other types of immune cells called neutrophils arrive at the site of CV inflammation as well. Neutrophils do the same thing as monocytes—they release an enzyme called myeloperoxidase or MPO.
Lab tests can show Lp-PLA2 and MPO in the blood. They allow measurement of the inflammatory process inside the wall of the artery. These neutrophils are specific to the inflammatory process within the arterial wall, so they are more specific to CV disease than some other tests for inflammation.
Interleukin 6 (IL-6)
An example of other inflammatory tests is for interleukin 6 (IL6).
Interleukins are pro-inflammatory cytokines and anti-inflammatory myokines (a type of cytokine released by skeletal muscle cells). It is a protein produced by various cells in the body. It is nearly always elevated with CV diseases but can also be elevated with other infections or autoimmune disorders, so we must take it into consideration with the other markers or tests for CV disease and inflammation.
Targeting Inflammation: A Missing Link in Heart Disease Treatments
Can the presence of inflammation provide a more urgent warning?
Yes. Inflammation provides an opportunity for an earlier and more urgent warning of an impending heart attack. If we can warn patients that their arteries are currently inflamed, they can better understand the urgency of the need to cool those arteries back to their normal state of homeostasis.
Treat the Inflammation, Not Cholesterol
Rudolf Virchow was well known as the father of 2 fields of medicine: pathology and social medicine. He described arterial inflammation over 150 years ago (Virchow, 1856).
But Virchow’s findings of arterial inflammation were largely ignored for over 100 years. Why? Perhaps it was because of the discovery that most arterial plaque contains oxidized LDL cholesterol.
That’s why in the past 60 years, we witnessed a misdirected focus on cholesterol. Many blame that on Ancel Keys and Keys’ red herring that the primary ingredient of arterial plaque is cholesterol (Carroll, 2016).
However, newer data from the 1990s began to showcase inflammation.
Inflammation was strongly associated with future vascular events, independent of the usual risk factors (Berk, 1990; Liuzzo, 1994). It can be measured by testing things like high-sensitivity C-reactive protein (hsCRP) or interleukin 6 (IL-6),
By 1997, Paul Ridker and others provided compelling inflammation data in the Physicians’ Health Study. Ridker and others showed elevated hsCRP levels in healthy subjects before first-ever vascular events (Ridker, 1997). They showed that CV inflammation can be a critical warning of imminent danger.
Although current US medical standards give hsCRP a minor recommendation (class IIb), committees are too conflicted to mount a coordinated response (Ridker, 2016). Part of this hesitancy may be tied to hsCRP’s lack of specificity. hsCRP levels are likely to spike during infections like the common cold, flu, or arthritis.
Just like the stress test, the hsCRP test is known for its false positives and negatives. (That’s why we recommend multiple tests that look for CV inflammation.)
Not to mention that too few doctors use this important bio-monitor, and only a few patients are aware of the CRP test.
Does This Mean the CRP Test is Useless?
No. This doesn’t mean CRP is useless. It just means that users need to understand what they are looking at when they see an hsCRP test result.
Right now, preventive standards are slowly de-emphasizing LDL and focusing more on a generalized risk assessment (including inflammation assessment). The ACC/ADA prevention standard now gives a moderate (IIb) value to hsCRP. There is also a growing acknowledgment of newer methods of plaque detection, such as the coronary calcium score.
Sadly, it’s still too early for the standards committee to adopt more definitive techniques like CT angiography and CIMT. Standards processes do take decades before they enact a significant change.
Familial Hypercholesterolemia: An Indicator of the Relative Importance of LDL
Familial hypercholesterolemia (FH) is a genetic disorder that results in the production of exceptionally high levels of LDL.
It’s underdiagnosed. Fewer than 1 in 200 have a diagnosis. And most families with FH cases remain undiagnosed and are unaware of their condition.
A patient with an LDL of 180 or above would be suspected to have FH. Genetic testing, although imperfect, can be considered for verification.
There are about 2,000 genetic variations that can cause FH, but genetic testing covers only a few. Those few variations account for only 80% of FH cases.
This means that a positive genetic test result can’t help the patient that much. Still, knowing there’s an FH gene in the family would help other family members understand the need for CV risk awareness and treatment.
Why did we talk about FH?
Because FH would help us understand the relative importance of LDL among CV risk factors. If LDL was the most potent driver of heart attacks and strokes, then patients with FH are likely to die younger, right?
That’s not the case, though. If LDL was the most critical driver of heart attacks, then FH risk wouldn’t be as easily managed. In fact, we can usually manage FH risk. The risk for FH patients is more of a decreased capacity to manage other risks (like smoking or prediabetes).
It appears that there are far more significant CV risk factors than just having high LDL levels.
Can We Delay Atherosclerosis and Inflammation?
Fortunately, yes, often by decades. As preventive lifestyles become more common than now, so will centenarians.
While many doctors still see plaque-laden arteries as a part of normal aging, a decades-old study proved that notion to be false. It’s called the China study. It looked at 50,000 Chinese field workers up to 80 years of age. The good news is that these workers had no plaque or inflammation (Campbell, 2006).
This landmark study should have proved beyond any reasonable doubt that atherosclerosis is not age-dependent (although there is a strong correlation in the US) but lifestyle-dependent.
In other words, what affects the amount of inflammation in our arteries and the amount of plaque which leads to plaque rupture and ultimately in heart attacks or strokes is what we eat, how active we are, our level of stress, and other lifestyle-related factors.
If you found this article helpful and want to start taking steps toward reversing your chronic disease, Dr. Brewer and the PrevMed staff are ready to serve you no matter where you’re located.
To find out more, schedule a consult here: prevmedhealth.com
References
American Stroke Association. Atherosclerosis and Stroke. American Stroke Association website. https://www.stroke.org/en/about-stroke/stroke-risk-factors/understanding-risky-conditions/atherosclerosis-and-stroke. Last reviewed December 5, 2018. Accessed November 15, 2020.
Babey SH, Wolstein J, Diamant A, Goldstein H. Prediabetes in California: Nearly Half of California Adults on Path to Diabetes. UCLA Center for Health Policy Research. March 10, 2016. Accessed November 14, 2020.
Berk BC, Weintraub WS, Alexander RW. Elevation of C-reactive protein in “active” coronary artery disease. Am J Cardiol. 1990 Jan 15;65(3):168-72. doi: 10.1016/0002-9149(90)90079-g.
Brewer F. How to Test for Cardiovascular Inflammation. PrevMed website. https://prevmedhealth.com/how-to-test-for-cardiovascular-inflammation. Accessed November 14, 2020.
Brewer F. Prediabetes: A Risk for Heart Attack & Stroke? https://prevmedhealth.com/prediabetes-a-risk-for-heart-attack-stroke. Accessed November 14, 2020.
Brewer F. Reducing Arterial Plaque – Is It Possible? PrevMed website. https://prevmedhealth.com/reducing-arterial-plaque-is-it-possible. Accessed November 24, 2020.
Campbell TC, Campbell TM. The China Study: The Most Comprehensive Study of Nutrition Ever Conducted And the Startling Implications for Diet, Weight Loss, And Long-term Health. 1st ed. Dallas, TX: BenBella Books; 2006.
Carroll AE. A Study on Fats That Doesn’t Fit the Story Line. The New York Times website. https://www.nytimes.com/2016/04/16/upshot/a-study-on-fats-that-doesnt-fit-the-story-line.html. April 15, 2016. Accessed November 14, 2020.
Centers for Disease Control and Prevention (CDC). New CDC report: More than 100 million Americans have diabetes or prediabetes. CDC website. https://www.cdc.gov/media/releases/2017/p0718-diabetes-report.html. Page last reviewed July 18, 2017. Accessed November 14, 2020.
Huang L, Chambliss KL, Gao X, Yuhanna IS, et al. SR-B1 drives endothelial cell LDL transcytosis via DOCK4 to promote atherosclerosis. Nature. 2019 May;569(7757):565-569. doi: 10.1038/s41586-019-1140-4.
Jaffer FA, Libby P, Weissleder R. Molecular and cellular imaging of atherosclerosis: emerging applications. J Am Coll Cardiol. 2006 Apr 4;47(7):1328-38. doi: 10.1016/j.jacc.2006.01.029.
Kraft J. The Diabetes Epidemic and You. Bloomington, IN.: Trafford Publishing; 2008.
Liuzzo G, Biasucci LM, Gallimore JR, Grillo RL, et al. The prognostic value of C-reactive protein and serum amyloid a protein in severe unstable angina. N Engl J Med. 1994 Aug 18;331(7):417-24. doi: 10.1056/NEJM199408183310701.
Meng S, Fang P, Yang X, Wang H. Monocytes and Macrophages in Atherosclerosis. In: Wang H, Patterson C, eds. Atherosclerosis: Risks, Mechanisms, and Therapies. Philadelphia, PA: John Wiley & Sons; 2015:141-153. doi:10.1002/9781118828533.
Oshima K, Haeger SM, Hippensteel JA, Herson PS, Schmidt EP. More than a biomarker: the systemic consequences of heparan sulfate fragments released during endothelial surface layer degradation (2017 Grover Conference Series). Pulm Circ. 2018;8(1):2045893217745786. doi:10.1177/2045893217745786.
Ridker PM. A Test in Context: High-Sensitivity C-Reactive Protein. J Am Coll Cardiol. 2016 Feb 16;67(6):712-723. doi: 10.1016/j.jacc.2015.11.037.
Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997 Apr 3;336(14):973-9. doi: 10.1056/NEJM199704033361401.
Virchow R. Phlogose und thrombose in gefassystem, gesammelte abhandlungen zur wissenschaftlichen medicin. Frankfurt-am-Main, Germany: Meidinger Sohn, 1856:458.