A mysterious COVID-19 condition observed among children in the UK was reported last April 2020.
Health Service Journal got hold of one alert sent to GPs, stating that “last three weeks, there has been an apparent rise in the number of children of all ages presenting with a multisystem inflammatory state requiring intensive care across London and also in other regions of the UK.”
This “mysterious” condition is like Kawasaki disease, a rare condition that affects children and involves inflammation of blood vessels.
Similar cases also sprang in the US, with 15 children hospitalized in New York in May. The condition is now named MIS-C (Multisystem Inflammatory Syndrome in Children), debunking the notion that young ones are less affected by SARS-CoV-2.
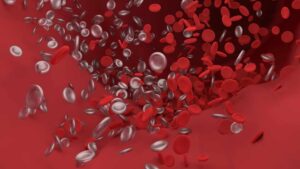
Adults also had their share of a “mysterious” condition. This time, it’s about excessive clotting.
In autopsies of a few patients who succumbed to COVID-19, instead of pneumonia and damage to the air sacs, there are tiny clots all over.
Broadway actor Nick Cordero is a popular example. In April, his right leg was amputated after suffering from clots that blocked blood from getting to his toes. He later died on July 5 at age 41.
MIS-C and the mysterious clotting in adults are just a few COVID-19-related complications that have not yet been fully understood. These conditions, though, have a common factor—inflammation.
Let’s briefly discuss inflammation and its connection to cardiovascular health, high sugar levels, and COVID-19.
1. The immune system is not always “friendly”
The discussion on inflammation starts with the immune system.
Our immune system is involved with the body’s process of injury repair. It kills, digests, and removes pathogens like viruses and bacteria.
Ironically, the immune system also creates inflammation while protecting the body. Rheumatoid arthritis is a common example where the immune system attacks joint tissue. Lupus, Hashimoto’s thyroiditis, and inflammatory bowel disease are other common inflammatory conditions.
The blood vessels are also a target of inflammation, as seen in the children with MIS-C and adults with excessive clotting conditions.
2. Inflammation causes heart attack and stroke
Cardiovascular (CV) inflammation starts with damage in the intima, the thin lining of the artery wall.
This intima has ample space not only for passing blood cells and nutrients but also for LDL cholesterol. And when LDL cholesterol gets trapped within those walls, this initiates plaque formation and build-up.
The immune system, however, senses arterial plaques as foreign matters.
It sends Immune cells called monocytes to the arterial walls, which now triggers an immune response. Monocytes turn into macrophages, then macrophages attack plaques similarly to how they attack pathogens. This process produces foam cells and fatty streaks, and both materials are inflammatory.
Simultaneous to the above process, other immune cells, enzymes, and cytokines are also attracted to the inflamed area, further increasing inflammation. This could weaken the arterial wall, specifically the thin fibrous cap that prevents any accumulated dead material from leaking into the bloodstream.
Over time, inflamed plaques could rupture like a pimple. If that happens, enzymes get released into the bloodstream, and this could activate platelets to form dangerous clots.
Clots could break off and get pushed into smaller blood vessels. Clots can also grow so large enough to stop blood flow completely. (This is one thing that seems to happen in adult COVID-19 patients with excessive blood clotting problems.)
That’s not all. Large clots can block blood flow to the tissue and kill it by cutting off the oxygen supply.
If the oxygen-starved tissue is in the heart, the result is a heart attack. If the tissue is in the brain, the result is a stroke.
3. Inflammation could be prevented
Fortunately, CV inflammation could be prevented or slowed down often by decades.
While many doctors still see plaque-laden arteries as a part of normal aging, a decades-old China Study (which looked at 50,000 senior Chinese field workers) proved that notion to be false.
This just shows that what affects inflammation, plaque build-up, and ultimately, heart attacks or strokes is our lifestyle—what we eat, how active we are, our stress level, and other lifestyle-related factors.
4. High sugar levels drive inflammation
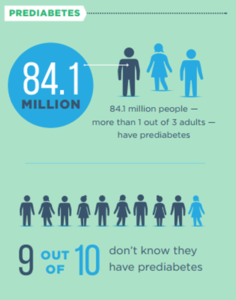
CV inflammation’s most common driver is having constant high sugar levels, as seen not only in diabetics but also in people with prediabetes.
Associated with aging or unhealthy fat stores, prediabetes can already increase plaque growth dramatically.
In 2017, the CDC said that around 84 million adults in the US have prediabetes. However, 90% of these people don’t know they are prediabetic.
As far as COVID-19 is concerned, one observed pattern is the increased risk brought by pre-existing conditions, including prediabetes and diabetes.
It’s not yet clear why COVID-19 presents a danger to prediabetics and diabetics. It’s also not fully understood how inflammation exactly works in COVID-19 patients and why people have varying reactions.
But the things that we already know can help every one of us take an active role in terms of our health.
If you found this article helpful and want to start taking steps toward reversing your chronic disease, Dr. Brewer and the PrevMed staff are ready to serve you no matter where you’re located.
To find out more, schedule a consult here: prevmedhealth.com