COVID-19—is it already a pandemic? Should we be concerned? What should we be doing? In this article, let’s do a basic rundown of a disease that’s gripping the world in early 2020.
COVID-19 vs. 2019-nCoV
Let’s tackle some definitions first. On February 11, 2020, WHO (World Health Organization) named the new disease COVID-19 (Corona Virus Disease 2019). It’s caused by the 2019-nCoV (2019 novel coronavirus), which was later officially named as SARS-CoV2 (severe acute respiratory syndrome coronavirus 2). The virus was named as it’s genetically related to the original SARS virus that broke out in 2003.
Some COVID-19 Facts
The intermediate hosts of the 2019-nCoV are still unsettled. However, a few candidate species are bats, pangolin (scaly anteaters), and civet cat. These species are a delicacy in China, as particularly seen in Wuhan’s meat markets where the virus was speculated to have originated. Such animal-to-human transmissions are no longer new. SARS, MERS, and Ebola had bats as their home species; the bubonic plague was transmitted by fleas from rodents to humans.
The Centers for Disease Control and Prevention (CDC) shared simple, practical facts about COVID-19, which you can see on CDC’s website.
- COVID-19 can make anyone sick. It’s not specific for the geographic location. It’s not specific for any age or ethnic group.
- The risk of COVID-19 in the US is currently low. People released from isolation did not pose a threat.
- People who have completed quarantine or released from isolation don’t pose a risk. (Quarantine is taking a whole population, like when China quarantined the entire city of Wuhan. Isolation is when persons are isolating themselves to decrease transmission to others.)
- COVID-19 can be prevented through simple means. Check the section on “How to protect yourself.”
- Some people are at increased risk of developing COVID-19, like people who have been in close contact with an infected person or stayed in an area with ongoing COVID19 spread.
Why is COVID-19 a concern?
WHO recently raised the danger warning of COVID-19 from high to very high. Why? One, the disease has a relatively high fatality rate. 2% is considered high, and COVID-19’s rate is currently at 3.4% as of March 9.
COVID-19 also has a high transmission—2-3 times per case. That means each individual case could cause 2 to 3 more infections. Not to mention that COVID-19’s spread appears to be of asymptomatic transmission. SARS and MERS (Middle East respiratory syndrome) did not have a lot of COVID-19’s qualities, and that’s why SARS and MERS ended up not being that much of a huge problem.
Johns Hopkins has a great interactive website that will show the number of cases and the spread of COVID-19 throughout the world. As of this writing (March 9), here’s the snapshot of the site:
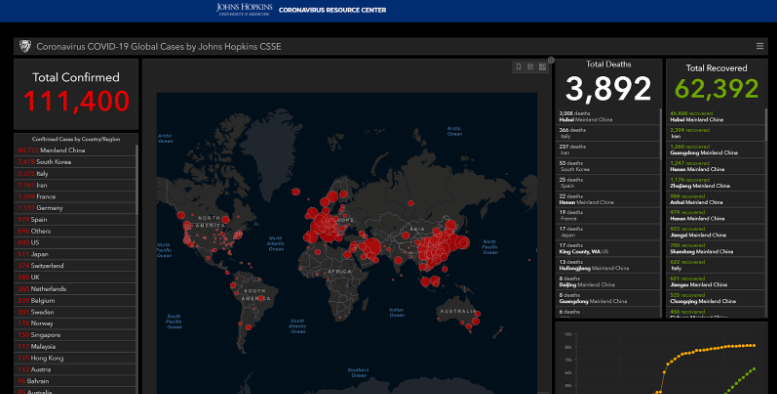
Confirmed cases have shot up to over 110,000, with cases concentrated in China at over 80,000. The next hotspots are South Korea, Italy, Iran, France, Germany, and Spain. The current tally for the US is at 603 cases. Now, total deaths are at 3,800+ (putting the mortality rate at 3.4%). The total recovered is at more than 62,000.
(After stopping short of declaring COVID-19 a pandemic in previous briefings, WHO announced the status on March 11.)
Comparing COVID-19 with other diseases
So, is COVID-19 going to be a threat? It could be. Let’s compare COVID-19’s fatality rate with that of other diseases.
- The seasonal flu is at 0.1%. (That’s one reason many are taking COVID-19 seriously.)
- SARS and MERS had higher fatality rates. 8-10% for SARS, and 36% for MERS. However, SARS and MERS didn’t spread as well as COVID-19, so they didn’t create many significant problems.
- The Spanish flu of 1918 has a fatality rate of 2%, around the same level as COVID-19. However, deaths are attributed to the Spanish flu’s high infection rate. It was easily spreadable, and it’s estimated that 30-50 million died with the Spanish flu.
- The bubonic plague, depending on the type, had a 15-100% mortality rate, wiping out up to 50% of some populations in Europe. This pandemic was dubbed the Black Death.
Here are a few reasons we didn’t immediately cover COVID-19. One, we’re having a huge epidemic in cardiovascular disease. We’re in the middle of it, and we think that’s all right. There are 2 heart attacks per minute in the US alone, with a 50% sudden mortality right for heart attacks. With strokes, every 40 seconds in the US alone, death occurs every 4 minutes, and about 25% of strokes lead to permanent disability.
Two, we worry too much about COVID-19 but not enough about flu. Flu takes more deaths and more disability in this season alone, though it doesn’t appear to be in a growth phase like that of COVID-19.
Check this video where we discussed in depth whether COVID-19 is indeed a pandemic risk.
Will summer stop COVID-19?
Most people say that once the summer hits, COVID-19 will dissipate. While that’s true with flu, and here had been some evidence that summer dissipated other coronavirus-type potential epidemics, it remains to be seen with COVID-19. In the US, one can still get the flu during the summer, albeit at lower rates. Another thing to think about is that tropical climates rarely have such type of seasonal transmission because these places don’t have seasons.
How does COVID-19 affect the lungs?
COVID-19 injures the lungs through inflammation, leading to what we call ARDS (acute respiratory distress syndrome). Air comes through the trachea or windpipe, which branches out into multiple sub-branches. At the end of the sub-branch is alveoli, little air pockets where the lung area aerates the blood. When we respire, blood rushes into the lung, goes past the alveoli, releases carbon dioxide, and then takes up oxygen.
The problem here is that inflammation fills these areas and creates a lot of liquid within the lungs, making the alveoli squeezed shut. When someone gets ARDS, they need help to breathe. They would get tired as they can’t pull their lungs open and pull all of those air sacks open.
How to manage ARDS
This slide from WHO talks about the ways doctors manage the inflammation in the lungs that are having ARDS.
- Intubating and putting pressure into the lungs. If the alveoli are left wholly closed, that could cause more damage. So doctors decreased the amount of flow and kept these alveoli inflated, and that act made a huge difference. The patient, however, won’t enjoy being intubated and will fight it. For successful intubation, the patient then has to be paralyzed.
- Putting the patient in a prone position (on their face) instead of being on their back. This helps drain some fluids.
How to protect yourself: Hygiene vs. exposure
Let’s go to the practical part—how to protect yourself.
Hygiene
- Hand washing: Wash hands with soap and water for at least 20 seconds.
- Avoid touching your eyes, nose, and mouth, especially with dirty or unwashed hands.
- Stay home if you’re sick.
- Cover any cough, or sneeze with a tissue paper, and throw away the tissue paper.
- Clean surfaces with regular household cleaner.
- N95 masks: Should we all wear N95 masks? It’s up for debate, but experts have been saying that N95 masks are not for people that are well. These are for the use of people that are already sick, isolate them, and protect the others.
Exposure
Apart from hygiene, this another way of protecting yourself. For now:
- Avoid traveling to China or places with travel restrictions to avoid contracting the virus and spreading it further.
- Avoid large meetings or public gatherings. For instance, in Paris, groups of 5,000 or more people are currently prohibited. Check for local guidance for churches and schools within your locality.
- Consider abandoning the custom of handshaking.
- In using facilities (like in gyms), consider wiping down the equipment, washing hands, or wearing gloves.
The bottom line is COVID-19 is not that big of a threat if we all take precautions and arm ourselves with proper knowledge. By knowing the signs, symptoms, and simple prevention, we can all help in stopping the spread of COVID-19.
If you found this article helpful and want to start taking steps toward reversing your chronic disease, Dr. Brewer and the PrevMed staff are ready to serve you no matter where you’re located.
To find out more, schedule a consult here: prevmedhealth.com