We once had a viewer by the name of Richard Dixon. Before Richard had a knee replacement surgery, he went through a pre-op exam. It was during that time that he discovered that he had calcified arteries around his heart.
Richard’s doctor put him on vitamin K2 MK7. That time, Richard knew little about the vitamin’s benefit. It was said, though, to be suitable for clearing plaque. Years after his knee operation, his X-rays showed he no longer had the dreaded calcium deposits.
With Richard’s pleasant experience with vitamin K2, he suggested that I check vitamin K2. In our YouTube channel, vitamin K2 proves to be one of the most popular topics.
For Richard’s story and the essential points that we initially highlighted about vitamin K2, you can find them in this video.
Vitamin K1 vs. vitamin K2
First, let’s differentiate vitamins K1 and K2. These are variants of vitamin K. Both are fat-soluble. Both act as a cofactor in certain processes involving osteocalcin and other bone proteins.
Now the differences.
Vitamin K1:
- Other names are “phylloquinone” and “phytomenadione.”
- It can be sourced from green, leafy vegetables.
- It’s involved with the coagulation process.
- It is also known as “menaquinone.”
- It has subtypes, from MK4 to MK13.
- The subtypes differ in chain lengths. (MK7 is the vitamin K2 variant Richard took.)
- It can be obtained from meat, eggs, cheese, and natto. (Natto is fermented soybeans, a Japanese food).
- It’s involved in tissue calcification, particularly in bones and arterial walls.
- Vitamin K2’s involvement with arterial calcification is why it’s a popular (albeit controversial) topic in cardiovascular (CV) health discussions.
Vitamin K studies
What does the scientific literature say about vitamins K1 and K2?
The studies on lab animals and humans, unfortunately, yielded inconsistent results. Much of the inconsistency, however, is because most research failed to differentiate vitamins K1 and K2.
Here are some examples:
- The Nurses’ Health Study: Around 40,000 nurses were involved. A moderate decrease in CV risk was found. However, researchers were looking at vitamin K1 here.
- Health Professionals Follow-up Study: This study is built on the same hypotheses of the Nurses’ Health Study. Here, there was no change in results in terms of vitamin K1.
- The Rotterdam Study: Researchers did both studies on vitamins K1 and K2. There were no changes seen with vitamin K1. On the other hand, researchers saw some decrease in CV risk with vitamin K2.
- The Beulens study: We’ll discuss this in the next section.
Vitamin K2 and calcium score
The study by Beulens and associates is an old one. It’s published in the Atherosclerosis journal in 2009.
The study involved 564 post-menopausal women. They were given a food questionnaire to estimate their intake of vitamins K1 and K2. 62% (360 women) got positive coronary artery calcium scores.
From the results, researchers analyzed the probability of calcification.
For vitamin K1:
- Researchers saw a relative risk of 1.17. That means there’s a 17% higher risk than average.
- In epidemiology, if the relative risk is 1, it means there’s no change.
- This implies that vitamin K1 provided no change.
- In short, there’s no decrease or increase risk of CV calcification.
For vitamin K2:
- The relative risk was 0.80.
- This implies that vitamin K2 lowers CV calcification. This was delightful news, though not earth-shaking at all.
- In short, a higher vitamin K2 intake appears to be connected with lower calcium scores.
Is it dangerous to have a high calcium score?
The calcium score is a gauge of the calcification level in the artery walls.
It will also show whether the arteries had already had inflammation in the past. Hence, a higher score means a person has undergone more cycles of inflammation than one with a lower score.
This makes calcium scan a good technique for screening plaque.
Can vitamin K2 remove plaque?
Here’s a question: Should we be concerned with calcified plaques?
At one point, no.
If you already had plaque, it’s better if it’s calcified and not soft. That’s because a calcified (hard) plaque is more stable. Calcification happens when the plaque is stabilizing.
What’s the most significant threat from having soft plaque? It’s inflaming a soft plaque, forming a deadly clot, and letting that clot cause stroke or a heart attack.
Another question: If you remove calcium from calcified plaque with vitamin K2, doesn’t that affect the plaque’s stability?
The answer is not simple.
If you asked us this question years ago, we would have said vitamin K2 may pull calcium out and destabilize a calcified plaque. It may (or may not) decrease CV risk.
So while vitamin K2 destabilizing calcified plaque seems like a quick and simple answer, there are emerging studies that do favors vitamin K2 for CV health.
That’s what we found out later.
Vitamin K2, MGP, and osteocalcin: New concepts
If you watched the earlier videos on vitamin K2, you’ll find that we weren’t that sold on supplementing with vitamin K2. That’s because of the notion that it could destabilize already calcified plaques.
Yet, viewers’ interest in vitamin K2 continues to increase!
Then in 2019, I encountered a book titled “Vitamin K2 and the Calcium Paradox.” It was written by Kate Rheaume-Bleue, a doctor of nutrition.
The book mentioned a thing called “osteocalcin” (among other things), which I was unaware of. This osteocalcin is said to impact both deposition and removal of calcium from bones, as well as diabetes.
So I checked vitamin K2 again.
Vitamin K2 affects several calcification processes
Before delving into osteocalcin, let’s first discuss matrix Gla protein (MGP). Like osteocalcin, MGP is one component that was missed in earlier videos.
Matrix Gla protein (MGP)
Here’s an illustration from an article in the Journal of the American College of Cardiology (JACC). The article’s title is “Changes in Renal Function in Patients With Atrial Fibrillation: An Analysis From the RE-LY Trial.”
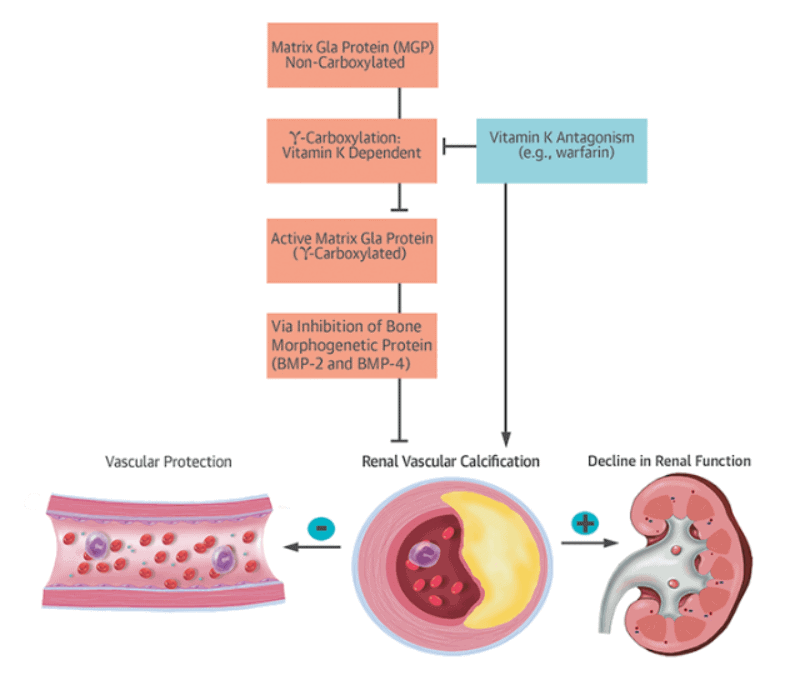
Here are the findings of the JACC study:
- The enzyme MGP inhibits vascular calcification and promotes decalcification.
- MGP depends on vitamin K to do such things. This means MGP has to be activated by vitamin K to do its job. The process is called “gamma-carboxylation.”
- If MGP is not carboxylated, it can’t help pull calcium out of the arteries.
- With this information, it seems vitamin K2 isn’t directly pulling out calcium in arteries. Instead, it activates MGP to do this feat.
What’s more:
- There are so-called vitamin K antagonists (like the anticoagulant warfarin), which can block vitamin K, stop gamma-carboxylation, and put MGP in the inactivated form.
- People on warfarin or any vitamin K inhibitor have been observed to have more calcification in their arteries.
- While we mentioned in the previous section that calcified plaque is better, in this JACC article, increased calcification led to arterial damage and a decline in renal function.
For an in-depth discussion on MGP, check this short video on the connection of vitamin K2 and MGP.
Osteocalcin
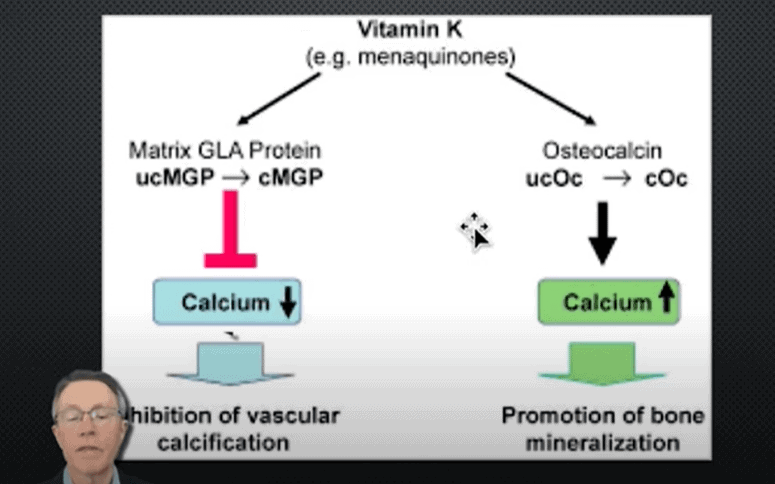
Now, osteocalcin.
Osteocalcin is a different enzyme. It does exactly the opposite of MGP. If activated, it increases calcification and promotes bone mineralization.
So carboxylated MGP pulls calcium out of the vascular area. On the other hand, carboxylated osteocalcin puts calcium into the bone.
However, to do their jobs, both MGP and osteocalcin have to be converted from an uncarboxylated to a carboxylated form. And carboxylation requires vitamin K2.
Vitamin K2 affects bone mineralization
Vitamin K2 isn’t only limited to activating osteocalcin and MGP. In this video, you can see that vitamin K2 also affects osteoclasts and osteoblasts.
What are osteoblasts and osteoclasts? These are 2 types of cells that control bone growth and density. Osteoblasts deposit bone calcium and protein for the bone to grow. Osteoclasts do the opposite.
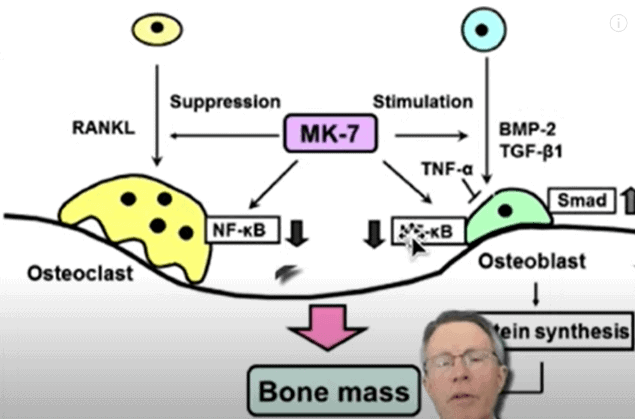
From the above image, see that vitamin K2 MK7 can stimulate osteoblasts or suppress osteoclasts. So even within the bones, vitamin K2 is involved in both processes of pulling calcium out of the bone and putting calcium into the bone.
Osteocalcin and diabetes
Aside from putting calcium into the bones, osteocalcin puts another angle to the vitamin K2 story. Let’s list first some studies:
- Reduced serum concentrations of carboxylated and undercarboxylated osteocalcin are associated with the risk of developing type 2 diabetes
- Osteocalcin is related to enhanced insulin secretion in gestational diabetes
- Association between serum osteocalcin and markers of metabolic phenotypes
- Low osteocalcin level is a risk factor for impaired glucose metabolism in a Chinese population
If you notice, all these studies mentioned osteocalcin along with insulin resistance or diabetes. These are signs that glucose metabolism is linked to osteocalcin. For instance:
- Osteocalcin levels in humans are inversely correlated with multiple various variables of type 2 diabetes, such as glucose intolerance and insulin resistance.
- Decreased levels of osteocalcin have been correlated with premature or myocardial infarction and coronary heart disease.
- Osteocalcin increases adiponectin, adipocytes, fat cells, and proliferation of beta cells.
- Osteocalcin increases insulin and insulin sensitivity. This leads to improved glucose handling and lower fat mass.
While we still don’t know the exact things going on, this is an interesting set of relationships.
Check the video below on osteocalcin and diabetes for further information.
Vitamin K2’s pleiotropic roles
Let’s get into an issue in biology called “pleiotropic roles.”
What does “pleiotropic” mean? It means that one thing is fulfilling multiple roles.
Take good old-fashioned Benadryl (an antihistamine) as an example. It has multiple uses. It is given as an anti-nausea drug, can induce sleep, and taken as an anti-allergy medicine (which is its most common use). It’s also taken for itching.
But does sleep have anything to do with allergy or itching?
At a glance, these Benadryl effects may seem unrelated until we go deeper. Things boil down to a thing called histamine. As an antihistamine, Benadryl blocks histamine then starts providing all these different pleomorphic roles or “side effects.”
Another example: statins. Doctors normally prescribe statins for cholesterol.
I usually don’t. When I recommend statins, it has something to do with a statin’s pleiotropic effect against CV inflammation.
Such must be the same thing with vitamin K2. Vitamin K2 appears to play lots of roles in terms of calcium activities, insulin resistance, and inflammation.
Takeaway
Vitamin K2 has few more effects and roles than we just don’t completely understand yet.
It affects both soft tissue (like artery walls) and hard tissues (like bones). Once vitamin K2 carboxylated MGP, that inhibits vascular calcification. Once vitamin K2 carboxylates osteocalcin, that increases bone calcification.
We also covered osteocalcin’s impact on insulin resistance and diabetes.
Vitamin K2 also affects osteoblasts and osteoclasts in distinct ways to customize the bone mass suited to the body’s current needs.
In a nutshell, vitamin K2 is very much involved in activating several components in managing not only calcium but also insulin resistance.
If you found this article helpful and want to start taking steps toward reversing your chronic disease, Dr. Brewer and the PrevMed staff are currently accepting patients for a limited time. Book an appointment here: https://prevmedhealth.com/
To ensure the quality of care, limited openings are available, so act quickly.
