In this week’s blog, I’m summarizing a really interesting conversation I had with Dr. Craig J Brown, about diabetic retinopathy. There are a lot of key concepts for you to digest and consider, if you already have insulin resistance and want to avoid some of the terrible complications of diabetes.
Dr. Craig J Brown has been working for over 40 years as an ophthalmologist. He’s performed over 9,000 cataract operations and thousands of ophthalmic laser operations; he has also been doing a lot of work specific to research in MTHFR supplementation (for people with genetic deficiency of the Methylenetetrahydrofolate reductase enzyme).
Dr. Craig also spent one year working in Northern Ghana, where he experienced a different culture of medicine where people died because they didn’t have $2.00 worth of antibiotics and malaria was in every corner.
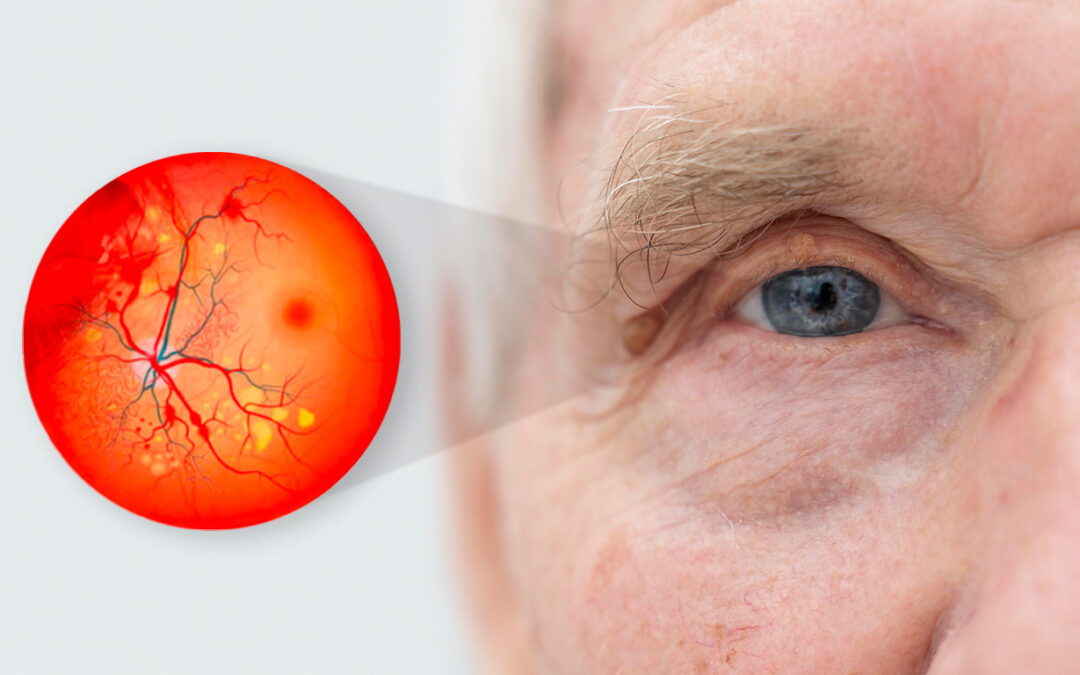
Dr. Craig defined diabetic retinopathy as a vascular disease caused by diabetes; it’s damage to the blood vessels of the eye. We should consider that the eye needs more food and oxygen than any other organ of the body. That’s why, when you faint or your heart stops, your vision goes first- and then your brain goes down next. There’s about 13 million diabetic retinopathy patients in the US, and half are undiagnosed. Eventually diabetic retinopathy leads to blindness, sooner if you have genetic defects like MTHFR malnutrition.
Most people over 50 have several risk factors; when diabetes receives a conventional treatment, blindness starts about 11 years after diagnosis. Poor lifestyles, nutrition and bad genetics make you more likely to get the complications of diabetes which are retinopathy, heart disease, peripheral neuropathy and kidney disease.
In ophthalmology there are two current treatments for diabetic retinopathy, we can burn two thirds out with the laser, resulting in loss of your side vision and night vision or we can stick a needle in the eye and inject expensive medications about every 6- 12 weeks. It seems to me, targeting lifestyle, diets and using products like Ocufolin are a good way for diabetics to get a lot more years before they need the needle or the laser, and maybe avoid it all together.
What about genetic predisposition for diabetic retinopathy? Well, if you don’t have a family history of macular degeneration, which is damage to the most important part of the retina, then I wouldn’t worry about it, but if you have people in your family that went blind from macular degeneration, then it’s a warning sign. You ought to do the things with the supplements, and the lifestyle that we know reduces macular degeneration. That’s a whole other discussion.
It is important to consider that there are two types of diabetic retinopathy: proliferative and non-proliferative. The initial stage is non-proliferative where you just have damage to the vascular endothelium (one of the layers of the vessels of the eye). You get profuse damage beginning at the stage of early pre-diabetes, then you begin to see loss of vascular density in the retina and decrease in blood flow.
Until now, it’s been considered an irreversible downhill trend. With ocufolin , we began to reverse the trend of blood flow, vascular density loss and diabetes. We started to move back towards normal.
Then there’s the proliferative stage when there are enough damaged blood vessels that you get capillary drop out, you get ischemia (lack of blood supply), you get nerve fiber layer infarcts and you start secreting vascular endothelial growth hormone, the body’s way of producing more blood vessels; new blood vessels grow and proliferate. The problem is that in the eye, they tend to rupture and bleed; the blood forms a scaffold that causes scar tissue, which normally is a good thing, but in the eye it causes detached retina.
They say the eye is the window of the soul. It’s certainly the window of the brain because the blood vessels of the retina and the retina itself embryologically come from the brain; when you’re looking at the retina, and you’re looking at the blood vessels of the retina, you’re looking at exactly the same blood vessels and tissue type, whatever is going on in the retinas is going on in the brain.
Dr. Wang, who is the principal investigator in our studies with ocufolin, just received a $1.4 million grant from NIH to correlate retinal blood flow with brain blood flow as part of a dementia push from NIH. I think you could say that diabetes causes vascular dementia. About half of the people that we saw have Alzheimers, really have vascular dementia.
If you put them on a lifestyle program, and you put them on ocufolin, you will see their cognitive function improve, their MRIs improve; In fact, there are a lot of people that don’t know they have pre-diabetes. They have what we call central nervous system diabetes, many of us know that insulin is a critical part of forming short-term and long-term memory.
The damage being done by unrecognized pre-diabetes and diabetes is just devastating.
If you found this article helpful and want to start taking steps toward reversing your chronic disease, Dr. Brewer and the PrevMed staff are ready to serve you no matter where you’re located.
To find out more, schedule a consult here: prevmedhealth.com
REFERENCES
1.- https://prevmedhealth.com/alzheimers-should-be-called-type-3-diabetes/
2.- https://prevmedhealth.com/prediabetes-a-risk-for-heart-attack-stroke/